
Sandra1 already had seven tattoos. Most of them were small. Lining her right outer thigh were six separate designs, the largest of which was about three inches in diameter. The seventh tattoo was more conspicuous, a First Nations bird on her right forearm, just above the wrist.
On her birthday in 2007, she wanted to get a new and unique neuron tattoo. Most of us are familiar with rods and cones, the classic retinal photoreceptors that transduce light into electrical impulses. Lesser known among the neurons in the retina are intrinsically photosensitive retinal ganglion cells (ipRGCs). These neurons express melanopsin, a light-sensitive protein involved in the production of melatonin, a hormone that regulates circadian rhythms (including the sleep-wake cycle). The ipRGCs project directly to the suprachiasmatic nucleus in the hypothalamus, the brain’s circadian pacemaker.
Sandra had a deep interest in circadian rhythms because of their significance in bipolar disorder (she had bipolar I disorder). Disruptions of the sleep-wake cycle are a prominent aspect of this condition. Before the existence of the f.lux® program that limits the amount of blue light emanating from your screen at night, before the studies demonstrating that electronic devices can suppress the production of melatonin (thereby altering your circadian clock), Sandra went out and bought yellow light bulbs for the lamps in the house. “But I can’t read in this dim yellow light!” I complained.
In preparation for the ipRGC tattoo session, I sent her several articles illustrating these rare neurons, which comprise only 5% of all ganglion cells in the retina. She chose an illustration from a 2005 Nature paper.
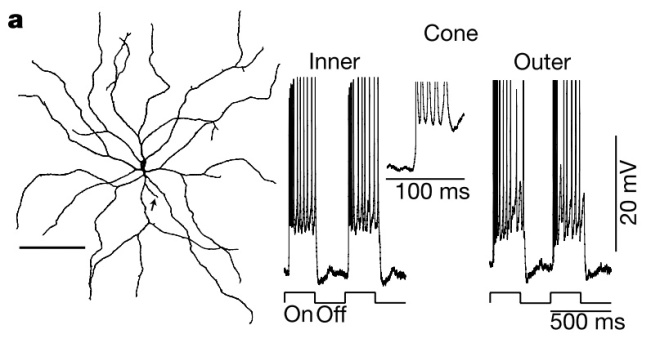 Modified from Fig 3a (Dacey et al., 2005). (Left) Drawing of a giant ipRGC cell (arrow indicates axon). The cell was recorded from the in vitro retina (“retina in a dish”) and then filled with a substance to visualize it. (Right) Electrical responses (voltage traces) of this cell to a specialized light stimulus.
Modified from Fig 3a (Dacey et al., 2005). (Left) Drawing of a giant ipRGC cell (arrow indicates axon). The cell was recorded from the in vitro retina (“retina in a dish”) and then filled with a substance to visualize it. (Right) Electrical responses (voltage traces) of this cell to a specialized light stimulus.
Most stereotypical neurons have a long axon, but this giant ipRGC does not (see arrow in Fig. 3a). Sandra wanted the tattoo to look like a standard neuron (and she enjoyed the idea of an axon running down her arm), so she had the artist embellish the drawing with an extra branch. She also had horrid arachnophobia, and did not want anyone to mistake this work of art for a spiderweb.
The results were quite impressive.

Then,
In 2007, [science writer] Carl Zimmer posed a question on his blog: are scientists hiding tattoos of their science? It turned out that many of them were, and they were willing to share their ink with him and the world.
Hundreds of people sent in their science tattoos. The original chronicle of this collection is nearly impossible to reconstruct from Zimmer’s many blogs, hosted by ScienceBlogs, Discover, National Geographic, Typepad, etc. Fortunately, the best of these tattoos were collected in a book called Science Ink: Tattoos of the Science Obsessed. Sandra was invited to submit a photo of her Neuron Ink.

Photo by Maurice Li.
In an entry called “Ganglion Cell”, Zimmer eloquently wrote:
It is sensitive to blue light, but it does not paint the blue of a bluebird. Instead, it sends its color elsewhere: to neurons that control the size of the pupil, to regions of the brain that set the body’s clock, to other regions that release hormones that make us sleepy and wakeful.
Sandra got two more tattoos after that, both in January 2016. One of these was the cover art from her book, Reliant.
Her very last tattoo was a daffodil to represent being a cancer survivor.

About this, she said:
Daffodils are the official flower of the Canadian Cancer Society and daffodil pins are sold each spring to raise funds. They’re the first flowers of the year, pushing through winter decay to burst forth with hope and life. A daffodil is a good symbol.
At the two year post-treatment milestone, the oncologist told her that the chance of recurrence was less than 5%. There was reason for optimism, because the doctors said she was cured. But six months later, after experiencing right upper quadrant pain, Sandra was diagnosed with stage 4 cancer. There was an 8 cm tumour in her liver that was “missed” because her ten prior scans didn’t bother to screen the most likely sites of metastasis.
The irony of her final tattoo was not lost on me.
On her birthday this year, I decided to get the same ipRGC tattoo (sans axon). It was my first; I did not have any tattoos before this.

I wish she was there with me to see it.
Footnote
1 Sandra Dawson, my late wife. See There Is a Giant Hole Where My Heart Used To Be.





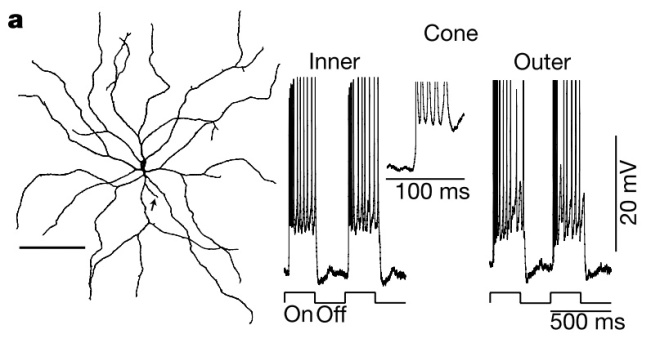 Modified from Fig 3a (
Modified from Fig 3a (









